Post-COVID: Why am I so tired?
Many of us have either now had COVID-19, had the vaccinations for them, and/or still fighting to not catch it. Many of us have also returned to our pre-COVID lifestyles including travel, increased work schedules, or simply socializing with friends again. Yay!
It is so nice to enjoy company again. I wish it wasn’t so hard for me to get there. I find that I am tired much more than I was before, and I just don’t have the motivation I used to have pre-COVID to call up my friends and ask them if they want to hang out. Sound familiar?
Even though we are all experiencing some sort of normalcy again – which is awesome – it seems like the activities that we greatly enjoyed before are just a bit harder to get ourselves to. We all seem a bit tired… all the time… especially if we are recovering from the virus.
If this sounds familiar, you are in the right place. Today I want to talk about post-COVID fatigue, how we got here, and how we are to get ourselves back to where we were before the pandemic. Let’s get happy again!
Post-COVID fatigue: Why am I so tired?
First off, it is super normal to feel tired after having a virus. When we first get a virus, our body goes into full superhero mode, increasing our immune response, filling up with antibodies, doing everything we can to fight the invader and make sure that it won’t come back. It is pretty cool that our bodies just know how to do this.
However, all that fighting on the inside makes us tired on the outside. We are using all our fuel to fight the bug, which is why our doctors tell us to rest, drink lots of fluids, and wait until we are feeling better before we return to our normal activities.
We fail to talk about the aftermath. After we have had a virus, it takes some time to get back to normal. We can feel 100%, but when we jump back into our crazy schedules our body seems to not function like it did before. All of a sudden, we feel tired after a long work day, a wedding, or a night of going out. More than we did before in fact. “But I already spent the time needed to recover,” we think, “why is this virus so hard for me to get over?”
Well, our bodies have never experienced this type of virus before. It is something completely foreign to us, and it takes time for our bodies to build up the antibodies we need to fight it. So, we might be feeling great after all that time resting, but in reality, our bodies are still hard at work.
Imagine for a second that you have never run a marathon, but you want to try. You prepare for it by training hard, then on game day you manage to run the complete the 42.195 km and you feel like a hero! The next day, would you expect to be able to go back to work full force without any fatigue? Doubt it. It takes time for our bodies to recover from a marathon, just like it takes time for us to recover from a virus.
But instead of taking the time to rest and recover post-COVID, we just jump right back into our lives – prolonging the healing process. This is why we feel tired. We are not giving our bodies the time they need to rest and recover from the marathon we just ran!
Post-Pandemic Fatigue: Why am I so tired?
“I haven’t had the COVID virus, so why am I tired?”
When our bodies go through a bout of stress, whether physiological (like from a virus) or psychological (like from having our lives turn upside-down for a couple years), a few things happen.
First, our body enters an acute stress response. In a way, this acute response allows our body to either fight the stressor or run away from the stressor with all our energy and strength. This is why most people call it our “fight or flight” response.
Biologically, our body activates two centres in our body. One is called the hypothalamic-pituitary-adrenal axis (or HPA axis for short), and the other is called the sympathetic-adrenal-medullary (or SAM axis). These axes influence multiple structures and organ systems within the body through the release of catecholamines and glucocorticoids to prepare the body for a fight-or-flight response (Sapolsky et al., 2000). The response sets the body up with all the tools it needs by involuntarily triggering physiological alterations that include increasing heart rate, blood pressure, respiration rate, and metabolic changes – all with the hopes to increase that amount of energy available to the body so it can fight with all it’s got, (Dusek & Benson, 2009).
This is an incredibly important process that has been passed down by generations to help our species survive. Back in the day when we were providing for ourselves as hunters and gatherers, back when food and shelter weren’t a given, sometimes predators, like tigers or bears, would hunt us. Our body’s ability to come together and give ample strength and energy to the areas in our bodies that needed it helped our species survive.
The problem now is that sometimes, in our 21st century world, that stressor doesn’t go away right away. Sometimes we go through a couple years of chronic stress. For 2 years (and maybe more) we have all been living in the unknown. For some of us this fear came with real life-or-death situations for ourselves or our family, and that can take a large toll on our bodies.
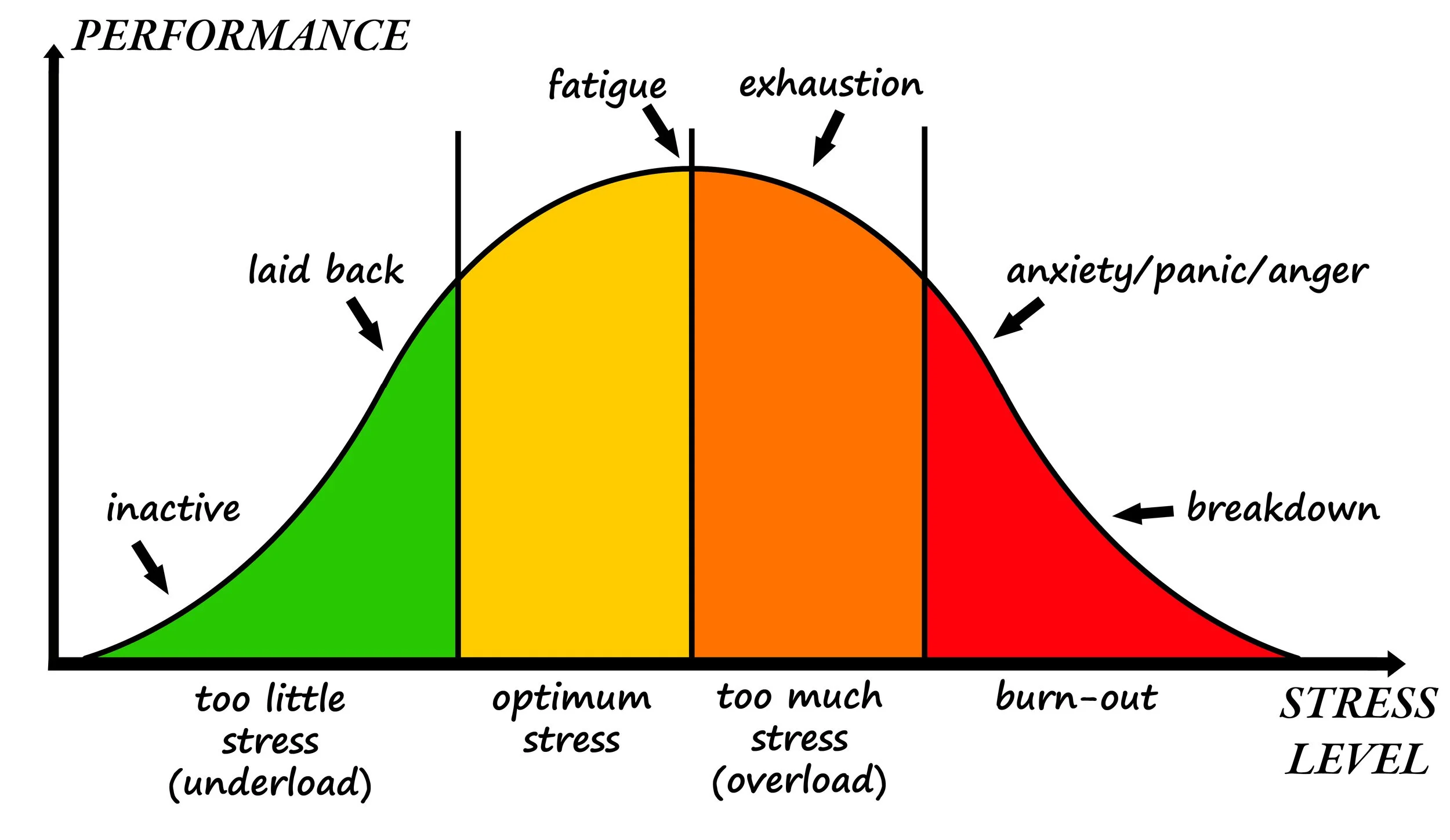
When our body enters a chronic stress response phase, our bodies start to form maladaptive alterations in our stress response, hormone levels, and allostatic load, (Juster et al., 2010).
Basically, our bodies try to adapt to a life where that stressor won’t go away and eventually goes into a state of over-adaptation (or as the doctors like to called “allostatic overload”). The over activation of that HPA- and SAM-axis eventually cause the whole system to collapse on itself, leaving us more depressed, inflamed, dysregulated, and more prone to stress-related diseases like high-blood pressure, diabetes, anxiety/depression, aging, dementia, and more – yikes! I like to call this phase wired-and-tired. “Wired” because we feel like we have a low threshold for incoming stressors and “tired” because we feel fatigued instead of energetic.
A group of doctors in the late 1990s and early 2000s figured out something pretty interesting about this whole phenomenon of chronic stress and allostasis, however. Apparently, the stressor is NOT the cause of this whole cascade effect (sorry everyone, we can’t blame COVID for this one), it is our individual differences in our brain’s interpretations of and reactions to stressors that the ultimate determinants of vulnerability towards allostasis or resilience against stress-related effects on the body – (for more information on this, check out the studies done by neuroscientist B.S. McEwen).
“How we perceive the stressor is the ultimate factor.” Interesting right?
Bonnie Henry had an amazing slogan for the first bit of the COVID-19 pandemic, “be kind, be calm, be safe.” What a great way for us to fight the effects of the pandemic. I love when something so simple, when explained, ends up being something incredibly profound. The more we fear, stress, freak-out, or react to all the craziness that has been happening over the last few years, the more the pandemic will have an influence on our body, mind, and health.
If you feel like you are in a situation that is over-your-head, it is wise to take a step back, take a few deep breaths, and simply follow the steps “be kind, be calm, be safe.” Everything will be ok eventually, you just need to wait for the cards to fall back in place.
However, there are a few other tips and tricks that you can do to help bring your body back into a state of homeostasis (or balance), where we have ample amount of room for stress without it sending us off into a spiral of allostasis. Let’s dive into that now.
What can I do to help this process along?
There are lots of things that you can do to help yourself get back to normal, and it starts with listening to your body and allowing it to take a break. It is ok if you feel like you need an afternoon nap for a while, or if you need to say “no” to a party that you were only going to out of obligation. It is ok to feel tired all the time, and it is ok to sleep for longer hours. We have all just been through a psychological and physiological roller coaster! It would be a miracle if we were able to just “pick up where we left off” without feeling some sort of fatigue. It is totally normal. Just keep drinking fluids, eat well, get into a light exercise regime, and sleep when your body wants to sleep and your body will reorganize itself in no time.
Want some more specific tools to help the recovery process along? Here are some ways that you can help your body get back to normal.
1. Osteopathic Manual Therapy
Osteopathic manual therapy (or OMT) has been shown in literature to have a balancing effect on the body. First, it improves the functioning of the autonomic nervous system, or in other words balances the body’s “fight or flight” response (or sympathetic response) with its “rest and digest” response (or parasympathetic response). Since we have all been running our fight-or-flight response for so long, rebalancing this system can have a great effect on our overall allostatic load.
OMT has also been shown to normalize hormone levels, improve heart rate variability, reduce perceived stress, and balance allostatic load (Abraham et al., 2021; Collebrusco et al., 2018; Dixon et al., 2020; Emmet et al., 2018; Fornari et al., 2017). This research suggests that osteopathy can be a non-intrusive form of treatment that could aid in the management of chronic stress symptoms alongside today’s more traditional methods of psychological support.
Chronic stress is also correlated to chronic pain, which is another way that OMT can help. If you want to learn more, you can book an appointment with one of our osteopathic practitioners at www.corepotentials.ca/appointments.
2. Balancing nutrition
There are a few vitamin and mineral supplements that can help your body get back to normal. You can find most of these by eating foods rich in these vitamins and minerals, which are easy to find with a quick google search, or you can take a supplement for a while until you feel like you can get it from your food.
Besides the obvious ones like vitamin C and vitamin D3 for immune support, there are a few others to look out for. For instance, the combination of a B-complex vitamin (especially one with B12 and folate) has been shown to boost mood and moral. Why is this important? Well, if you are feeling better or more positive, you will have more motivation to get back to your normal routine. Zinc is also a powerful tool for hormone regulation (which is important post-stress) and immunity.
The biggest factor however is optimum hydration to allow your body to filter and expel all the toxins and hormones that you have accumulated during this time. It is usually recommended to drink at least 8 cups of water a day. One of the questions I get from my clients is “how big of a cup?” My answer is usually the same: “If you are a big person, then big cups, and if you are a small person, then small cups.” We can get hung up on the specific amounts of all the nutrients that we are trying to take in, and I find that it creates a stress all on its own - so just do your best to get in what you can. You can also increase your protein (especially vegetable protein like lentils, peas, or beans with healthy grains) to support your body’s detoxification, re-building, and balancing processes.
During these hotter days don’t forget to replenish not only your H2O, but all your electrolytes as well for optimal functioning. This includes calcium, magnesium, sodium chloride (or salt), and potassium.
3. Re-introducing exercise (especially cardiovascular)
Mild exercise has been shown to decrease the effects of stress on the body. You start producing hormones like endorphins that allow you to think happier, and you flood the prefrontal cortex of your brain with more blood, reforming pre-COVID pathways of logical thinking and reduced perceived stress. You look better which gives you a sense of pride, your pain decreases which helps you not feel so crappy all the time, your heart rate and blood sugar normalize, and so much more. Starting up an exercise routine post-COVID is a great way to get your body to jump-start back to health, just keep in mind to start small so that you don’t add more physiological stress. Baby steps are all you need.
4. Clinical counselling
I can’t stress this category enough. We all need someone that we can talk to that is not our mom, cousin, work-friend, or anyone else that has influence in your life. Someone that is completely unbiased, where you can be vulnerable and say the things that are on your mind without the fear of your thoughts coming back to bite you. Someone who is trained to help support your through all the changes and stresses that have happened and continue to happen since COVID started. Taking the plunge and reaching out for that support can be the best way to help us rebalance our stress (both physiological and emotional). Remember how I said that the biggest factor of allostasis (or our bodies getting knocked off by stressors) is not the stressor itself, but how we individually interpret and react to them. Our perceived stress is the only thing that matters, and clinical counselling is an excellent way to come up with tools to help us perceive in a more positive light.
5. Energy medicine
Another great avenue to help with post-COVID fatigue is energy medicine. Energy medicine focuses more on how our stressors (again whether physiological like catching a virus or psychological like the emotions attached to the pandemic itself) effect our subtle energy (or “bioenergetic field” in western science). All dis-ease starts in our energetic field, and it is important for us to recognise the potential that energy medicine has to help rebalance our body from its root issue. I am no expert in energy medicine, but I highly respect how it helped me as I went through my osteopathy schooling, starting my own business, and the stress that came with the COVID pandemic shutting us down for a while. When I get a treatment from Becca, our energy medicine practitioner, I simply feel more balanced. I am able to think straight, sleep better, and feel more alive - like myself again. It is also a great way to rebalance yourself after a hefty session with your counsellor.
Our September Newsletter will have a story about Becca’s journey in catching COVID and using energy medicine to support her through the process.
That’s all folks! Make sure to subscribe to our newsletter if you want to be notified when our next blog comes out. All our practitioners greatly enjoy getting to share our experiences and knowledge with you. I hope you enjoyed this one. Until next time!
Warm Regards,
Britte Nielsen, DOMP, RHN.
Disclaimer: The information on this site is provided as an information resource only, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any health care decisions or for guidance about a specific medical condition.
References:
Abraham, C., Sloan, S. N. B., Coker, C., Freed, B., McAuliffe, M., Nielsen, H., Riscoe, T., Steele, R., Dettwiler, A., Oberley, G., Zaremski, K., Joy, K., Selby, A., Wells-Lewis, R., & Creamer, B. A. (2021). Osteopathic Manipulative Treatment as an Intervention to Reduce Stress, Anxiety, and Depression in First Responders: A Pilot Study. Missouri Medicine, 118(5), 435–441.
Collebrusco, L., Fabri, S., Furfaro, A., Tanini, I., Lombardini, R., Rizza, A., & Zavarella, P. (2018). Osteopathy and Emergency: A Model of Osteopathic Treatment Aimed at Managing the Post-Traumatic Stress—Brief and Useful Guide—Part 2. Health, 10(11), 1597. https://doi.org/10.4236/health.2018.1011120
Dixon, L., Fotinos, K., Sherifi, E., Lokuge, S., Fine, A., Furtado, M., Anand, L., Liberatore, K., & Katzman, M. A. (2020). Effect of Osteopathic Manipulative Therapy on Generalized Anxiety Disorder. Journal of Osteopathic Medicine, 120(3), 133–143. https://doi.org/10.7556/jaoa.2020.026
Dusek, J. A., & Benson, H. (2009). Mind-Body Medicine. Minnesota Medicine, 92(5), 47–50.
Emmet, D., Nuño, V., & Pierce-Talsma, S. (2018). OMT to Address the Physiologic Effects of Stress. Journal of Osteopathic Medicine, 118(2), e11–e11. https://doi.org/10.7556/jaoa.2018.028
Fornari, M., Carnevali, L., & Sgoifo, A. (2017). Single Osteopathic Manipulative Therapy Session Dampens Acute Autonomic and Neuroendocrine Responses to Mental Stress in Healthy Male Participants. Journal of Osteopathic Medicine, 117(9), 559–567. https://doi.org/10.7556/jaoa.2017.110
Juster, R.-P., McEwen, B. S., & Lupien, S. J. (2010). Allostatic load biomarkers of chronic stress and impact on health and cognition. Neuroscience & Biobehavioral Reviews, 35(1), 2–16. https://doi.org/10.1016/j.neubiorev.2009.10.002
McEwen, B. S. (1998). Stress, Adaptation, and Disease: Allostasis and Allostatic Load. Annals of the New York Academy of Sciences, 840(1), 33–44. https://doi.org/10.1111/j.1749-6632.1998.tb09546.x